FDA Approved Parkinson's Drug Treatments:
The following are a list of drugs approved to treat the symptoms of Parkinson's disease, primarily "Motor Fluctuations". Note that none of the drugs approved by the FDA for treating Parkinson's disease are not cures, nor do they slow down or halt the progression of the disease. By contrast, there are many drugs in development and drugs in clinical trials which hold hope for such a treatment. Currently the most popular treatments for Parkinson's are the Levodopa based drugs blended with Carbidopa to improve longevity of the drug in one's system. There are four classes of drugs used to control dopamine for the treatment of Parkinson's disease: Levodopa, Dopamine Agnosts, COMT inhibitors and MAO-B inhibitors. Some are used alone or in combination to gain the synergystic benefits. The drug's effects are often refered to as "On time", where the drugs take effect vs "Off time", when the drug effects are wearing off and less effective.
Drugs are refered to by their "corporate brand name" and by their "generic name".
Levodopa:
Levodopa is a drug supplied to the brain so that motor neurons can produce dopamine to counter the deficiency caused by Parkinson's disease. Levodopa is combined with other drugs like Carbidopa to improve half life, absorption and efficacy. Carbidopa prevents the conversion of Levodopa into dompamine while in the blood stream so that levodopa can make the journey to the brain for conversion to dopamine where it is needed. When high doses are taken, the peak medication levels of Levodopa may produce involuntary movements known as dyskinesia. Another condition is dystonia, when your muscles continuously contract (cramping), which may cause parts of your body to twist or toes to curl. This leads to repetitive movements or abnormal postures (for example curling of the toes or turning of the foot or ankle) and can cause great pain and discomfort. Both dyskinesia and dystonia are more prevelent at peak doses.
Levodopa has the ability to cross the blood-brain-barrier to reach the aflicted nigral dopaminergic neurons. Levodopa is the precursor used by the body to generate dopamine within the nigral neurons in the brain (by a reaction with aromatic amino acid decarboxylase - ACC), which then acts as a neurotransmitter.
Protein consumption can inhibit the efficacy of Levodopa absorption so it is best to time the intake of protein-rich foods around the intake of Levodopa and reserve protein-rich foods for dinner. As a general guideline, take Levodopa a half hour before meals or one hour after meals (or longer for protein rich meals).
Various versions of Levodopa based drugs exist. Here a list of the popular Carbidopa/Levodopa solutions:
- Sinemet: also available in a Sinemet "Controlled Release" (CR) version.
Studies have shown that patients on Levodopa have a higher risk (2 to approximately 6 times higher) of developing melanoma. ref FDA: page 6
Side effects can include halucinations, diskenesia, dystonia and sudden onsets of sleep. - Crexont: a carbidopa and levodopa based oral medication formulated with immediate release (IR) and extended release (ER) pellets designed to kick in at two rates and last longer. Claims to need 3 doses per day rather than the typical 5 per day.
- Rytary: a carbidopa and levodopa based oral medication formulated with time release beads designed to kick in more quickly and last longer. New dosage must be calculated and not directly interchangeable with prior Sinemet dosage.
- Stalevo: a carbidopa, levodopa and entacapone based oral medication
- Duopa: a gel formulation which is slowly and continuously pumped through a tube inserted surgically through the stomach into your intestine to smoothly delivers medication.
Bypasses stomach for quick and direct absorption. Typically disconnected at night.
Support group and patient mentor program: Duopa Mentor - Inbrijia: inhaled levodopa. Can be used up to 5 times a day. Low rate of diskinesia. Quick acting (10 - 20 minutes) - improved motor scores after 30 minutes.
Similar to an asthma inhaler.
Side effects: cough, upper respiratory tract infection, nausea, discolored sputum. Dangerous side effects if taken with MAO inhibitors. - Vyalev: (Abbvie) subcutaneously, continuously (24 hr) pump infused foscarbidopa/foslevodopa (carbidopa/levodopa). Claims to improve on time by 1.75 hrs per day.
- Onapgo: (Supernus Pharmaceuticals) subcutaneous, continuously (24 hr) infused (by a wearable pump) apomorphine (dopamine agonist - works by stimulating dopamine receptors).
Tip: drink lots of water with every dose to help push it along from the stomach to the first part of the intestine when it can be absorbed. Levodopa does not get absorbed in the stomach (ref).
Also see Mid Stride - probably the best resource on carbidopa/levodopa drugs.
Levodopa Side Effects and Risks:- Long term motor complications of levodopa: clinical features, mechanisms, and management strategies (2004)
[PDF]
- Ref pg 3 of PDF: "It is shown that untreated patients do not develop dyskinesia even if their disease is advanced and that a prolonged period of levodopa treatment is needed to produce dyskinesia in MPTP-exposed primates"
- Ref pg 4 of PDF: "After five years of levodopa therapy, nearly 50% of patients develop motor complications and after 10 years nearly 100% of patients are affected by them"
(ref: Recognition and treatment of response fluctuations in Parkinson's disease 2002) - Ref pg 4 of PDF: "Unfortunately, once established, these complications can be resistant to medical therapy"
- Ref pg 4 of PDF: "With disease progression, the useful anti-parkinsonian effect of each levodopa dose lasts a progressively shorter time. Patients have to use levodopa more frequently for relief from parkinsonian symptoms. They find that the dose that used to give them relief from their motor symptoms for several hours is now effective for progressively shorter periods"
- Problems with long-term levodopa therapy for Parkinson's disease (1994)
- Homocysteine and Parkinson's disease: A dangerous liaison? [pdf] (2007)
- "Hyperhomocysteinemia has been repeatedly reported in PD patients; the increase, however, seems mostly related to the methylated catabolism of L -Dopa"
(Hyperhomocysteinemia: a medical condition characterized by an abnormally high level of homocysteine in the blood. Homocysteine is a known inflammation marker and plays a role in the pathophysiology of neurodegenerative disorders.)
- "Hyperhomocysteinemia has been repeatedly reported in PD patients; the increase, however, seems mostly related to the methylated catabolism of L -Dopa"
- Elevated Plasma Homocysteine Levels in Patients Treated With Levodopa (2003)
DOI: 10.1001/archneur.60.1.59- "patients with Parkinson disease (PD) may have elevated homocysteine levels resulting from methylation of levodopa and dopamine"
- "Mean plasma homocysteine levels were 31% higher in levodopa-treated patients"
- Higher vitamin B12 level at Parkinson's disease diagnosis is associated with lower risk of future dementia (McCarter et al, 2020)
"Higher levels of serum vitamin B12 at PD diagnosis correlate with lower risk of future dementia."
"This duration range was chosen to limit the impact of levodopa treatment, which has been associated with increased homocysteine levels and lower vitamin B12 levels," - FDA report on Sinemet - see page 6 for melanoma risks

MAO-B (Monoamine Oxidase-B) Inhibitors:
(early treatment) antidepressant therapeutic agents for panic disorder and social phobia. Believed to prevent the breakdown of dopamine in the brain and may help protect the brain from the progression of Parkinson's. MAO-B inhibitors can worsen the side effects of Levodopa. Targets MAO-B thus affecting dopaminergic neurons. MAO-B is a protein which enables the break-down of excess dopamine thus inhibiting MAO-B allows for more dopamine to be available thus helping Parkinson's patients. MAO-B is also a participant in the production of GABA in astrocytes (nutritional bridge between the blood supply and neurons) which is involved in stress and neurotransmitter inhibition leading to dormant neurons. Thus a MAO-B inhibitor reduces GABA, stress and neurotransmitter inhibition. Reversible inhibitors of monoamine oxidase A (RIMAs) are a subclass of MAO-B inhibitors and are considered to be a safer alternative (ref). MAO-A is also known to affect carcinogenesis.
When taking a MAO-B inhibitor it is best to avoid foods high in tyramine such as cheese, aged meat, smoked fish, dry sausages, sauerkraut, miso, or other fermented or aged products, as it can contribute to high blood pressure. MAO-B inhibitors have a mild effect on Parkinson's disease motor functions and is used in early or moderate Parkinson's disease patients.
- Selegiline (Eldepryl, Zelapar): also known by its chemical name, L-deprenyl, treats depression. Makes low dosage Levodopa more effective by preventing the dopamine from being destroyed.
Lower dosage of Levodopa avoids its side effects.
Can be used alone to delay Carbidopa-Levodopa treatment by about a year.
Also used as an anti-depressant.
Slight stimulant like properties can cause insomnia.
- An interim report of the effect of selegiline (L-deprenyl) on the progression of disability in early Parkinson's disease. The Parkinson Study Group (Shoulson, 1992)
"We conclude from these preliminary results that selegiline (10 mg/day) delays the onset of disability associated with early, otherwise untreated PD." - The effect of deprenyl (selegiline) on the natural history of Parkinson's disease (Tetrud, Langston, 1989)
"Therefore, early deprenyl therapy delays the requirement for anti-parkinsonian medication, possibly by slowing progression of the disease."
DOI: 10.1126/science.2502843
- An interim report of the effect of selegiline (L-deprenyl) on the progression of disability in early Parkinson's disease. The Parkinson Study Group (Shoulson, 1992)
- Rasagiline (Azilect, Azipron): Teva. Used in early and moderate Parkinson’s to reduce motor fluctuations. Mild effect on Parkinson's motor functions.
Designed as a newer replacement for selegiline based therapies.
Studies have found it to slow the progression of Parkinson's.
May cause hallucinations and psychotic-like behavior or induce sudden unconsciousness.
Phase 1 drug trial results: NCT01879748 (2013)
Also see:- Increased survival of dopaminergic neurons by rasagiline (Finberg et al., 1998)
"The protective action of rasagiline on dopaminergic neurons, even under stringent serum-free conditions, is striking, ..."
DOI: 10.1097/00001756-199803090-00026 - Rasagiline adjunct therapy in patients with Parkinson's disease: post hoc analyses of the PRESTO and LARGO trials (Elmer, 2013)
"Rasagiline was an effective first adjunct therapy in levodopa-treated patients; benefited patients with signs of early "wearing off"; improved all cardinal PD symptoms; and further improved symptoms in patients already receiving other adjunctive dopaminergic treatment."
DOI: 10.1016/j.parkreldis.2013.06.001 - A Double-Blind, Delayed-Start Trial of Rasagiline in Parkinson's Disease (ADAGIO study, 2009)
"Early treatment with rasagiline at a dose of 1 mg per day provided benefits that were consistent with a possible disease-modifying effect ..." - Longer Duration of MAO-B Inhibitor Exposure is Associated with Less Clinical Decline in Parkinson's Disease: An Analysis of NET-PD LS1 (Hauser et al., 2017)
"Our analysis identified a significant association between longer duration of MAO-B inhibitor exposure and less clinical decline."
DOI: 10.3233/JPD-160965
- Increased survival of dopaminergic neurons by rasagiline (Finberg et al., 1998)
- safinamide Xadago): FDA approved 2017 for treatment of "off" periods. Used with levodopa and carbidopa.
Dopamine Agonists:
In general medical terms, an agonist is a drug which can combine with a receptor on a cell to produce a physiologic reaction typical of a naturally occurring substance. The drug acts along a normal and natural pathway.
A dopamine agonist acts like dopamine by performing the same communications neurotransmitter function in the brain. Dopamine agonists are believed to work by making brain cells more receptive to dopamine. Dopamine agonists may be given alone or in combination with Levodopa/Carbidopa. Levodopa is often added if the patient's symptoms are not being controlled adequately. Side effects include hallucinations, excessive daytime sleepiness, dizziness, fainting, impulse control disorder (not recommended for those with addiction or gambling problems) and increased risk for heart problems. Dopamine agonists are effective in prevention and treatment of motor complications. Often the initial drug of choice in young and biologically fit older patients. Daytime excessive sleepiness can make this class of drug dangerous for those operating a motor vehicle. This class of drug may have bad withdrawal effects known as Dopamine Agnonist Withdrawl Syndrome (DAWS). Withdrawl symptoms include anxiety, panic attacks, irritability, fatigue, sweating, nausea, vomiting, restless leg syndrome, temperature dysregulation and pain.
- Pramipexole (Mirapex): used alone or with Levodopa. Reduces risk of dyskinesia but more addictive than traditional carbidopa-levodopa and may induce drowsiness.
Also see: Mirapex vs. carbidopa-levodopa - Ropinirole (Requip): has escalation of dosage issues, Reduces risk of dyskinesia with long term use
- Rotigotine (Neupro): transdermal patch
Also see the phase 1 trial NCT02055274 intramuscular injection version of this drug - Apomorphine (Apokyn, Ixense, Spontane, Uprima): also a treatment for opiod addiction. Apomorphine is not an opiod. Used to reduce L-DOPA dosing and reduce "off time". Injected. Check drug interactions.
- Kynmobi (Sublingual apomorphine): strip placed under tongue. Apomorphine activates both D2-like and, to a much lesser extent, D1-like receptors. May cause nausea and dizziness and may require taking an anti-nausea pill. Has to be titrated in doctor’s office (dosage tests required).
- Tavapadon: partial dopamine agonist targets only D1 and D5 dopamine receptors, potentially reducing unwanted effects such as loss of impulse control.
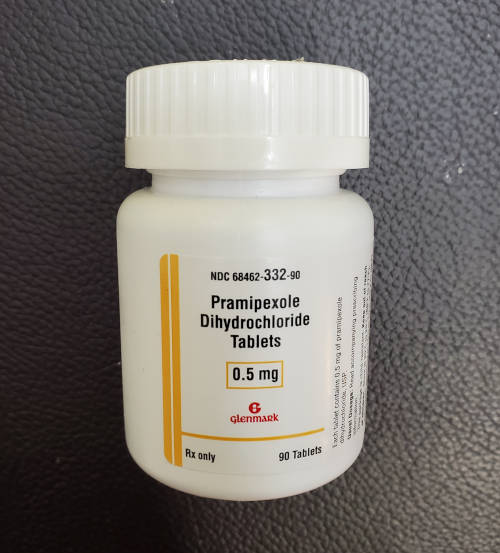
Pramipexole (Mirapex)
COMT (catechol-O-methyltransferase) Inhibitors:
COMT (catechol-O-methyltransferase) is an enzyme which degrades dopamine. Drugs listed here are used to block COMT so that dopamine is retained. Used with Levodopa to make it more effective by inhibiting the break-down of dopamine.
- Opicapone (Ongentys): extends effectiveness of Carbidopa-Levodopa (Sinemet) "on" time by about an hour. Common side effects are dyskinesia, constipation, increased blood creatine kinase, hypotension/syncope, and decreased weight.
Dosage: once daily
Side effects: dyskinesia, constipation, hypotension/syncope, weight decrease - Entacapone (Comtan): extends effectiveness of Carbidopa-Levodopa by inhibiting COMT from breaking Levodopa down, thus increasing the amount of Levodopa that reaches the brain, making Levodopa effective at significantly lower doses
- Tolcapone(Tasmar ): demonstrated significant liver toxicity (hepatotoxicity), which has led to its suspension
Rho-kinase inhibitors:
- Fasudil: Rho-kinase inhibitor and vasodilator. Fasudil, considerably lowered α-synuclein aggregation in an H4 cell culture model. More typically used to treat ALS.
A2A Receptor Antagonists:
The Adenosine A2A receptor has been shown to interact with Dopamine receptor D2. The Adenosine receptor A2A can be used to decreases activity in the Dopamine D2 receptors thus affecting dopamin flow.
- Istradefylline (Nourianz): oral medication to reduce "off" time by approximately 0.73 hours.
Dosage: once daily
Side effects: dyskinesia
Non-Motor Parkinson's Treatments:
Non-motor symptoms include uncontrolled movements such as dyskinesia, audible and visual hallucinations and dilusions, dementia, depression and various anxieties.
Dyskinesia Treatments:
Used to treat the side effects of high doses of levodopa. Dyskinesia will eventually affect those with Parkinson's disease given time.
Prevalence of dyskinesia for Parkinson's patients:- 8%: 7-12 months
- 26%: 2 years
- 40%: 4-6 years
- 90%: 10 years
- Amantadine ER (extended-release) (Gocovri, Symadine, Symmetrel, Osmolex ER): increases dopamine release and blocks dopamine reuptake to reduce levodopa induced dyskinesia.
Typically used with Levodopa based medicines.
A weak antagonist of the NMDA-type glutamate receptor (anesthesia effects) and can cause dizziness, and hallucinations.
Origionally developed and FDA approved as an anti-viral drug as a prophylactice agent against Asian influenza.
Dosage: once nightly
Side effects include dry mouth, dry eye, irritation of eyelids (blepharitis), nausea, decreased appetite, insomnia, orthostatic hypotension, constipation, visual hallucinations. - Pridopidine (Huntexil): is a dopamine stabilizer that interacts with dopamine D3, adrenergic α2C and serotoninergic 5-HT1A receptors. Primarily used as a drug to treat Huntington's disease.
- Clozapine (Versacloz, FazaClo, Clozaril): antipsychotic used to treat dyskinesia and also used to reduce the risk of suicidal behavior in adults with schizophrenia or similar disorders.
Hallucinations:
Hallucinations, both audible and visual, are often the side effect of Levodopa based medications especially for those with advanced Parkinson's who are taking high doses.
- Pimavanserin (Nuplazid): used to treat hallucinations and delusions in people with Parkinson’s
- Quetiapine (Seroquel): used to treat hallucinations and delusions in people with Parkinson’s
- Clozapine (Versacloz, FazaClo, Clozaril): antipsychotic used to treat hallucinations
Anticholinergics:
Anticholinergics are used to restore the balance between the two brain chemicals, dopamine and acetylcholine, by reducing the amount of acetylcholine. When dopamine levels drop, the levels of acetylcholine, another neurotransmitter, rises. Anticholinergics can impare memory and thinking and therefore rarely prescribed today. Hallucinations have been reported.
- Benztropine mesylate (Cogentin): used together with other medicines to treat the symptoms of Parkinson's disease (muscle spasms, stiffness, tremors, poor muscle control). Also used to treat a form of restlessness known as akathisia.. Benztropine may cause weakness or the inability to move particular muscle groups, especially in large doses.
- Trihexyphenidyl (Artane): used together with other medicines to treat the symptoms of Parkinson's disease.
Acetylcholinesterase Inhibitors:
This class of drug treats dementia by increasing the levels of acetylcholine in the brain.
- Rivastigmine (Exelon): used to balance two brain chemicals, dopamine and acetylcholine, by increasing the neurotransmitter acetylcholine.
Tremor Treatment:
Tremors fall into two categories:
- Action tremors: happpen when engaging muscles to hold a position.
- Resting tremors: occur when body part is at rest.
- Inderal, Hemangeol, Inderal, InnoPran (Propranolol): tremor treatment as well as blood pressure, angina, atrial fibrillation. Classified as a beta blocker.
Propranolol Reduces Parkinson's Tremor and Inhibits Tremor-Related Activity in the Motor Cortex: A Placebo-Controlled Crossover Trial (2024, Anouk van der Heide et al)
"The clinical implication of our findings is that propranolol could be a useful additional treatment option for PD tremor, whether or not it is triggered by stress, particularly for tremor responding insufficiently to dopaminergic drugs."
"propranolol is effective in reducing PD tremor across both stressful and resting conditions." - Mysoline (primidone): fast acting essential tremor treatment. Classified as a beta blocker.
Other:
- Nuplazid (pimavanserin): treatment for Parkinson's related hallucinations and delusions associated with Parkinson's dementia related psychosis or Parkinson's medications. Takes 4-6 weeks to take action.
- Northera (Droxidopa): used to treat orthostatic hypotension (dizziness upon standing up) in people with Parkinson's. Common for 40-60% of Parkinson's patients and a frequent cause of falls. Not to be taken close to bedtime as it can elevate blood pressure when laying down.
- Xeomin (IncobotulinumtoxinA): used to treat Sialorrhea (excessive drooling). Injection reduces saliva production and provides relief for about 3-4 months.
Avoid:
Drugs known to block or inhibit dopamine flow must be avoided as they may bring about symptoms of Parkinson's.
These include:- Dopamine Receptor Blockers:
- neuroleptics (including atypical neuroleptics)
- metoclopramide
- Drugs that reduce dopamine release:
- tetrabenzine and other VMAT2 inhibitors
Medications To Be Avoided Or Used With Caution in Parkinson’s Disease
Pros:
- Carbidopa-Levodopa based drugs have a long track record of reducing tremors in Parkinson's patients.
Cons:
- Carbidopa-Levodopa based drugs only mask symptoms, do not change the rate of progression of the disease, nor do they cure Parkinson's and they often have bad side effects.